
Ed. note: This is cross-posted on the CMS blog. See the original post here.
We’ve known for a long time that an ounce of prevention can be worth a pound of cure. Yet our health care system doesn’t always encourage prevention, especially around unmet social needs. These problems can lead to poor health that requires expensive emergency room visits or hospitalizations. Many social needs, such as housing instability, hunger, and interpersonal violence, affect individuals’ health yet they may not be detected or addressed during typical, short doctor’s visits. Over time, these unmet needs may increase the risk of developing chronic conditions and reduce one’s ability to manage these conditions, resulting in increased health care utilization and costs, such as emergency room visits or hospitalizations.
Perhaps we could interrupt the cycle of unmet social needs leading to illness in the first place. To explore this opportunity, the Department of Health and Human Services this week announced a new funding opportunity of up to $157 million to fund “bridge organizations” that will ask all their Medicare and Medicaid patients about health-related social needs, and then help refer them to community resources, assign “community health navigators” to help them connect with resources, and help communities themselves become healthier.
Here’s a hypothetical example of how the bridge might help: a mother comes in to a participating community health center for her child with asthma. During a complete social screening, the center learns the mother has been living in a moldy trailer after fleeing a violent home life. They refer the family to a local safe housing program and legal aid to protect her. The center also connects her with these services with the aid of a community health navigator. By helping the family find safe permanent housing, we reduce the frequency of the child’s visits to the ER for asthma attacks.
The five-year model, called the Accountable Health Communities Model, is the first Centers for Medicare & Medicaid Services (CMS) Innovation Center model to focus on the health-related social needs of Medicare and Medicaid beneficiaries.
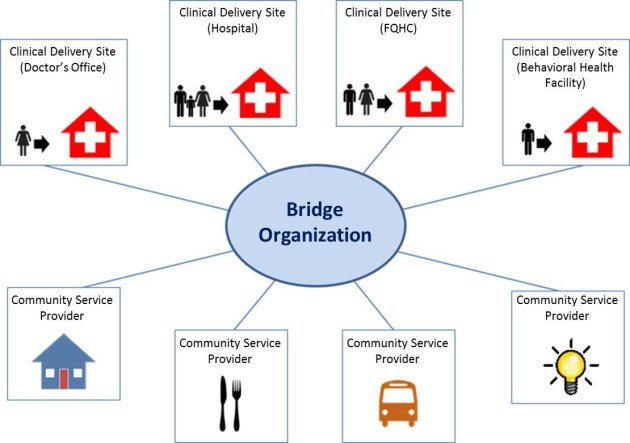
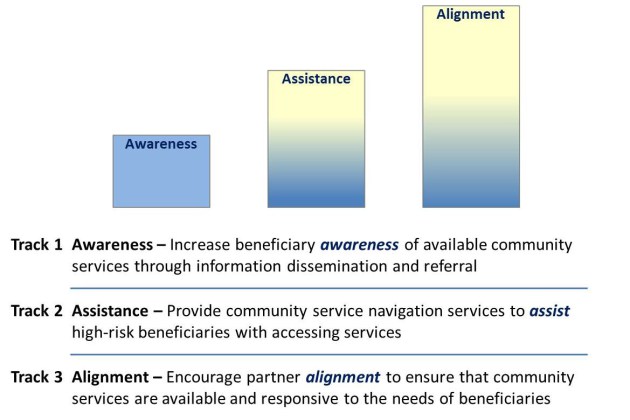
The model will test three scalable approaches to addressing health-related social needs and linking clinical and community services – community referral, community service navigation, and community service alignment. Bridge organizations will inventory local community service providers and furnish referrals to those agencies as needed. A total of 44 sites will be selected to provide intensive community service navigation, such as in-depth assessment, planning, and follow-up until needs are resolved or determined to be unresolvable for high-risk beneficiaries. Over the five year period, we’ll see if the bridge organizations help reduce total health care costs, emergency department visits, and hospital stays, and improve the quality of care.
To learn more about the Accountable Health Communities Model please visit: https://innovation.cms.gov/initiatives/ahcm.

