Chapter 2. Seek Early Intervention Opportunities in Health Care
Chapter Table of Contents
Introduction
The devastating impact substance abuse has on individuals, families, and communities is visible to most Americans; however, less visible but still significant is the impact substance abuse has on the healthcare system. Medical professionals spend a great deal of their time and resources treating patients with injuries and illnesses that resulted from substance abuse. Unfortunately, health care providers often do not have the training or resources to identify and treat patients’ underlying issues of substance abuse. Health care providers can play a crucial role in reducing drug use and its consequences. Health care providers must have the education and sufficient training to identify substance use problems and get patients the treatment they need.
The Affordable Care Act Includes Substance Use Disorder Services as an Essential Health Benefit The Affordable Care Act, signed into law by President Obama in March 2010, includes substance use disorders as one of the ten elements of essential health benefits. This is significant because it means that all health insurance sold on Health Insurance Exchanges or provided by Medicaid to certain newly eligible adults starting in 2014 must include services for substance use disorders. By including these benefits in health insurance packages, more providers can offer and be reimbursed for these services, which will result in more individuals being able to access treatment. The specific substance abuse services that will be covered are currently being determined, and will take into account evidence on what services allow individuals to get the treatment they need and put them on a path to recovery.
Principle 1. Catching Substance Use Disorders Early Saves Lives and Money
Screening, Brief Intervention, and Referral to Treatment (SBIRT)
It is critical for medical professionals to be able to identify the early signs of substance abuse in their patients and to intervene early. These early interventions can result in savings to the healthcare system and, most important, saves lives. SBIRT is a tool that enables health care professionals to ask patients about substance use during routine medical visits. SBIRT helps healthcare providers identify individuals with problems related to substance use, provide medical advice to help patients who have been identified as having risky substance use to understand the related health risks and consequences, and refer patients with more severe substance use-related problems to treatment
A number of Federal agencies, including SAMHSA, HRSA, the CDC, and the Indian Health Service (IHS), have incorporated SBIRT into many of the healthcare settings they support. In 2011, the IHS will introduce, in six Indian Health Service Emergency Departments and six Tribal Emergency Departments, an SBIRT model (tailored toward Native populations) to address substance use disorders. HRSA made costs related to SBIRT a fundable activity that requires annual reporting for Federally Qualified Community Health Centers. It expects as many as 260 of its health centers to participate. (Action Item 2.1A)
Reducing substance use through SBIRT is one way of providing healthcare professionals with the tools necessary to speak to patients about their substance use and help them get the treatment they need. One study on the use of SBIRT in Washington State showed a reduction in total medical costs and inpatient hospital costs (see inset).
Washington State Expands Services and Reduces Healthcare Costs: Treatment Expansion Initiative In 2005, the State of Washington expanded drug and alcohol treatment for individuals receiving Medicaid or state disability benefits. This expansion covered the integration of substance use disorder treatment into primary healthcare settings. The state Medicaid agency found that providing services for substance use disorders in healthcare settings reduced overall healthcare costs:
- Prior to the initiative, medical costs for disabled Medicaid clients with substance use disorders were rising much faster than the medical costs for Medicaid clients without substance use disorders (11 percent compared to 8.5 percent annually).
- Since the initiative, medical costs have been growing more slowly for clients with substance use problems compared to clients without substance use problems (2.8 percent compared to 4.7 percent
- annually).
- Expansion of treatment services in 2006 through 2009 yielded $107.4 million in savings. For every dollar the State spent, it is estimated to have saved two dollars in future healthcare costs.
SBIRT in Colleges and Universities
Underage drinking and substance use among college students threaten not only the present well-being of millions of students, but also our Nation’s future capacity to maintain its leadership in the fiercely competitive global economy. Studies have shown that drinking and substance use are a significant problem on our Nation’s college and university campuses. Nearly 4 million college students age 18 to 22 reported binge-drinking in the past 30 days, and 20 percent reported past-month use of marijuana or other illegal drugs.
While the problem is significant, use of SBIRT in campus health centers has shown promising results. Notably, a study funded by SAMHSA and conducted by the University at Albany – State University of New York found that SBIRT programs in campus health centers can help address college drinking. At a 6-week follow-up, students reported decreased alcohol use, more accurate perceptions of other students’ drinking, and increased use of strategies to enhance self-esteem and self-worth. Results of the study also indicate that changes in alcohol use were positively correlated with changes in perceptions of drinking among peers. This year, ONDCP in partnership with Education, will disseminate information on SBIRT to campus health centers and school administrators and provide university officials with screening tools and information on substance use that can be accessed on the schools, websites and in orientation materials by both parents and students.
School-Based SBIRT in New York City Public Schools
Since fall 2010, the New York City Health Department has been working to implement and integrate two SBIRT approaches in public high schools. Last December, 125 trained counselors in New York City’s Education Department were stationed in 75 public high schools. These counselors began delivering “Teen Intervene,” an evidence-based, multi-session intervention program. Although it is too early for formal evaluation of the program, preliminary reports from the field are positive. The NYC Health Department is implementing an SBIRT approach in five licensed school-based health centers. In these settings, a universal screening will be administered by clinical staff, and SBIRT services can be billed to health insurance. If the model is successful at these test sites, it will be implemented at all 45 school-based health centers in New York City. In schools where both of these SBIRT approaches are implemented, students with greater severity scores may be referred to the “Teen Intervene” counselor for the intervention component.
Families Referred to the Child Welfare System
Of children ages 3 and younger, 30 percent had drug abuse of parent(s) as one of the reasons identified for removal from home. Of children between the ages of 4 and 8, 25 percent of cases cited drug abuse of parent(s) as a reason for removal. Because of the connection between substance abuse and child welfare involvement, ONDCP has begun to collaborate with HHS’ Administration for Children, Youth, and Families (ACYF) on finding opportunities to get families the treatment they need without having children enter the foster care system.
ACYF has been working collaboratively with other HHS agencies to address the co-occurrence of substance abuse and child abuse and neglect. Along with SAMHSA, AYCF supports the National Center on Substance Abuse and Child Welfare, which builds knowledge about effective, family-focused practice and provides technical assistance. The Center also provides significant support to 53 recipients of Regional Partnership Grants, administered by ACYF. These grants support and enhance a region’s capacity to meet the range of needs for families involved with substance abuse and child welfare.
One area of collaboration between ONDCP and ACYF is exploring the use of assessments by child welfare workers to evaluate families who have been referred to the child welfare system. If substance abuse and other issues families are facing are properly identified and treated, parents will be more equipped to provide the care, love, protection, and support that all children need. Assessors screen families for issues related to substance abuse along with a host of other issues (such as domestic violence and other mental health problems). After the family has been screened, the assessor, in collaboration with a child welfare worker, refers families to interventions and treatment that holistically address the entire family’s needs. This approach allows families to stay unified and avoids placement of children into the foster care system, while providing families with the services they need.
Expanding the Addiction Medicine Workforce
Providing tools such as SBIRT is one way of helping current medical professionals properly address issues of substance abuse. However, it is equally important to train future health care professionals on substance abuse issues and provide current healthcare professionals with additional training about the complex nature of the disease of addiction, especially in light of the parity requirements contained in the Affordable Care Act. Education and training will become even more important in the coming years. It is anticipated that by 2020, approximately 7,000 addiction medicine doctors will be needed to care for an estimated 27 million patients who are dependent on substances.
Addressing the needs of these patients requires an expanded workforce of doctors, physicians’ assistants, counselors, nurses, and social workers. Work across the Federal government has begun to address the growing demand for an expanded work force. In particular, HRSA and SAMHSA established a technical assistance and training center to train healthcare providers on behavioral healthcare services, including substance use disorder services. HRSA and SAMHSA are aiming to increase the number of trained healthcare professionals. (Action Item 2.1C)
In addition, the Department of Labor established a grant program in 2011 that allows community colleges to compete for funds to expand and develop programs for substance abuse counselors and address the need for these professionals in this field. NIDA’s Centers of Excellence for Physician Information have developed curriculum resources on substance abuse and addiction that can be integrated into existing curricula to enhance medical student/resident physician education. These curriculum resources address pressing issues facing physicians today, in particular recognizing risk factors for, as well as identifying prescription drug abuse in their patients.
Along with increasing the specialization of providers in behavioral health, all doctors should have a baseline understanding of the disease of addiction. In 2010, ONDCP collaborated with the National Board of Medical Examiners to identify areas for improved substance use disorder content in the United States Medical Licensing Examination (USMLE). As a result, the USMLE will include a broader range of questions on substance use disorders and their relationship with other health conditions. Inclusion of these questions signals the importance of this knowledge to the practice of medicine, suggests that students need to master this material, and underscores the need for schools to include it in their curricula. (Action Item 2.1C)
Enhancing the psychological and behavioral health of military families was the first identified priority in the Presidential report, Strengthening our Military Families, which is designed to provide a comprehensive strategy to improve and expand substance abuse prevention, treatment, and recovery services available for active duty Armed Forces, the National Guard, and the Reserves.
New Action Item: Identify and Make Available Additional Training in Evidence-based Practices for Substance Use Disorder Assessment and Care to Healthcare Professionals Providing Care to Military Health System Beneficiaries. [DOD]
DOD will identify and make available additional training in evidence-based practices for substance use disorder assessment and care to healthcare professionals providing care to Military Health System beneficiaries. Additional training integrated into existing professional training and available online will make it more likely that providers can identify substance use disorders when present and can institute or refer for further care based on evidence-based principles.
Electronic Health Records
In 2009, the Health Information Technology (HIT) for Economic and Clinical Health Act (HITECH, Title XIII of the American Recovery and Reinvestment Act) funded several programs allowing doctors to accurately document patients’ complete medical histories, including the development of electronic health records (EHRs). EHRs will allow for the integration of substance use disorder treatment records into a patient’s medical records, thereby permitting the exchange of substance use information among medical professionals when appropriate, and with a patient’s consent.
Unfortunately, many health professionals who serve those with substance use disorders do not routinely use electronic health records. This presents a significant hurdle to integration of substance use disorder care into the primary care system. Without electronic health records, providers and their patients are not connected to statewide health information technology systems, and reimbursement for health services. To address this issue, the Office of the Assistant Secretary for Planning and Evaluation at HHS developed a web-based guide on providing services to certain vulnerable populations. The guide provides an explanation to providers on how to be included in state health information exchange activities.
While electronic health records can help improve care and reduce costs, there are concerns about privacy and security. In 2010, the Office of the National Coordinator for Health Information Technology at HHS established an advisory committee to develop health information technology and electronic health records that protect patients’ privacy and can be linked to the larger health information technology system.
Protecting patient privacy is especially important for individuals with substance use disorders because of the stigma often attached to these disorders. A person’s substance abuse treatment records remain confidential unless they sign a release, or unless a court order and a warrant are issued. If a patient is referred to treatment by the criminal justice system and signs a consent for disclosure, the patient cannot revoke the consent until he or she is no longer under the jurisdiction of the justice system. ONDCP will work throughout 2011 with Federal partners to disseminate updates, announcements, and developments surrounding the national infrastructure for Health Information Technology to prevention, treatment, and recovery service providers.
Massachusetts Screening, Brief Intervention, and Referral to Treatment (MASBIRT) Program Impacts
Clinic Practice and Patients’ Lives
Health Promotion Advocates in three urban hospitals and five community health centers in the greater Boston area used MASBIRT to screen more than 130,000 patients for unhealthy substance use and conducted more than 22,500 brief interventions within healthcare settings between 2007 and 2010. Medical providers realize substance use can have a significant impact on health, but they are often overwhelmed by competing clinical demands. Dr. John Knight at Children’s Hospital in Boston cited lack of time, lack of training, triaging competing concerns, lack of treatment resources, and unfamiliarity with screening tools as challenges he and other providers face when addressing substance use. MASBIRT is an approach that has made it possible for medical professionals in Massachusetts to do screening for unhealthy substance use in real time. “As a primary care pediatrician, I witnessed MASBIRT becoming a natural part of our clinical practice. Using MASBIRT, we have been able to get valuable information from patients about the extent of their substance use and what triggers their use. For example, during conversations with patients about substance use, it is often discovered that patients have mood disorders or exposure to violence, often in their relationships. As the medical provider, I am able to address the root causes of substance use. Using MASBIRT, in my opinion, is a satisfying approach for both the patient and the physician.” —Susan Gray, MD, a Primary Care Provider
Principle 2. Curb Pharmaceutical Abuse While Preserving Medical Benefits of Pharmaceuticals
Prescription drug abuse is the Nation’s fastest-growing drug problem. While there has been a marked decrease in the use of some illegal drugs, such as cocaine, data from the National Survey on Drug Use and Health (NSDUH) show that nearly one-third of people aged 12 or over who used illicit drugs for the first time in 2009 began with non-medical use of a prescription drug.66 Additionally, the latest MTF study—the Nation’s largest survey of drug use among young people—showed that prescription drugs are the second-most abused category of drugs after marijuana.
The epidemic warrants a significant public health response. Accordingly, in April the Administration released the Prescription Drug Abuse Prevention Plan titled, Epidemic: Responding to America’s Prescription Drug Abuse Crisis. The complete plan can be found here:
http://www.whitehousedrugpolicy.gov/prescriptiondrugs/
Preventing the misuse and diversion of prescription drugs while ensuring the availability of these important medications for those who have a medical need for them, requires a multi-pronged approach that includes prescriber and patient education, monitoring systems, disposal, and enforcement strategies.
HHS’s Behavioral Health Coordinating Committee (BHCC) has a subcommittee specifically dedicated to preventing prescription drug misuse.
Prescription Drug Monitoring Programs
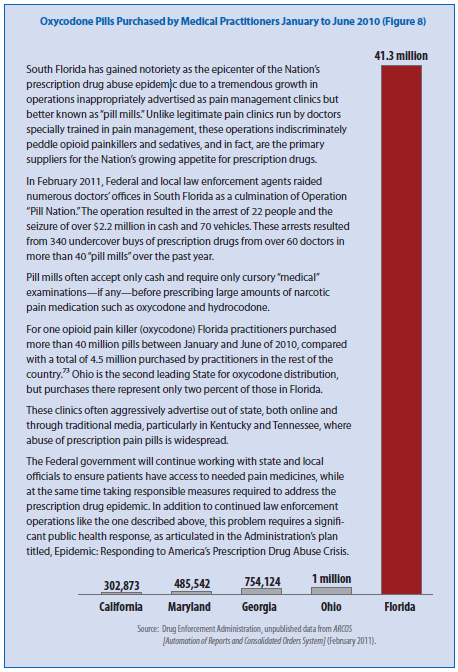
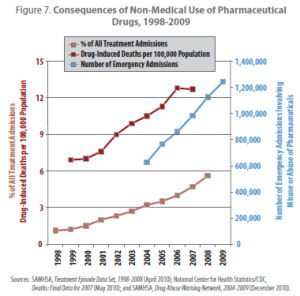
The easy availability of prescription pain medications and the misconception they are safer than illicit drugs, even if taken improperly, have led to dramatic increases in prescription drug abuse, overdose, and addiction. Nationally, an estimated seven million people aged 12 or older reported having used prescription drugs non-medically in the past month in 2009. Between 1998 and 2008, there was a four-fold increase in treatment admissions for individuals age 12 or over reporting abuse of prescription pain medication. In addition, CDC reports that the number of drug-induced deaths involving opioid pain medications more than tripled between 1999 and 2006, exceeding those from heroin and cocaine combined.
Prescription Drug Monitoring Programs (PDMPs) are a way to combat the misuse of prescription drugs and the harmful consequences associated with them. PDMPs are statewide electronic databases of dispensed controlled substance prescriptions that help healthcare providers identify prescription drug misuse. These medications are monitored because, in addition to their beneficial medical uses, they have abuse potential. Currently, 48 states have authorization to establish and operate a PDMP: 34 are operational. The structure, location within state government agencies, and the kinds of information PDMPs collect vary from state to state.
Legislatures in Georgia, Maryland, and Arkansas have recently passed legislation to institute PDMPs. However, there are states that remain without this helpful tool to help reverse prescription drug abuse trends. Without PDMPs, a state can become a haven for illegal drug diversion and drug-seeking behavior.
PDMPs can help in the delivery of comprehensive health care in many ways. For example, a PDMP can help pharmacists and prescribers support access to legitimate medical use of controlled substances. PDMPs can also help identify, deter, and prevent prescription drug abuse. They also have the capability to identify those with a substance abuse problem and facilitate an intervention and treatment. PDMPs can also assist regulatory and law enforcement authorities in identifying sources of diversion of abused pharmaceutical drugs. The usefulness of PDMPs has been supported by a Government Accountability Office (GAO) report. This report indicated that the PDMPs in Kentucky, Nevada, and Utah reduced unwarranted prescribing.
While the success of PDMPs has been documented, many states unfortunately still do not have programs in place. Of the 10 states with the highest number of prescriptions for OxyContin at the time of the GAO study, only two had PDMPs. Further, a recent study found that when Ohio’s PDMP data were used in an emergency department, providers changed the clinical management in 41 percent of cases. In cases of altered management, the majority (61%) resulted in fewer or no opioid medications prescribed than originally planned, whereas 39 percent resulted in more opioid medication than previously planned, indicating the database’s usefulness as a clinical tool to the doctor.
Because of the significant potential PDMPs can have in curbing abuse and helping link those in need of treatment, the Federal government is providing funds to support PDMPs. In 2010, the Bureau of Justice Assistance (BJA) administered the Harold Rogers Prescription Drug Monitoring Program (HRPDMP), which made grant funding available to states to plan for, implement, and enhance prescription drug monitoring programs. In future budget proposals, funding for these activities are included in other DOJ budget components. BJA also continued its work with the nonprofit IJIS Institute to develop standards for state PDMPs in sharing prescription drug data across state borders, to prevent doctor-shopping and drug diversion. Ohio and Kentucky PDMPs will be initiating real-time data exchange in 2011. (Action Item 2.2B)
In 2010, additional support for PDMPs came from SAMHSA, which oversaw the National All Schedules Prescription Electronic Reporting (NASPER) program. Under NASPER, states can apply for grants to support the establishment and improvement of their PDMPs. NASPER is a formula-based grant program that requires states to have a plan for interoperability and meet specific requirements for electronic standards and data reporting. To qualify for funding, states must also have a plan for information security and access. (Action Item 2.2B)
On October 12, 2010, President Obama signed the Secure and Responsible Drug Disposal Act into law. This law directs the Attorney General to develop rules making such disposal of controlled substances safe, easy, and affordable. As a result, fewer drugs will be available for diversion.
In 2010, DEA held the first National Take-Back Day, resulting in the safe and proper disposal of 121 tons of unwanted or expired medications nationwide. A subsequent event in April of 2011 netted 188 tons for safe and proper disposal at the 5,361 take-back sites that were available in all 50 states. This is 55 percent more than the 121 tons the public brought in during the September 2010 event. Because youth report that the prescription drugs they abuse come primarily from friends and family, activities that help adults remove expired or unneeded medications from their home are critical to abuse and diversion prevention efforts. These events also help educate adults about the importance of properly securing medications in their homes. (Action Item 2.2C)
Getting rid of unused or expired medication is one step to combating prescription drug abuse, but it must be coupled with education of medical professionals about proper prescribing. SAMHSA is helping train physicians about the importance of proper prescribing practices for opioids, which are routinely prescribed to relieve pain. Topics include doctor-shopping (the practice among some patients of seeking prescriptions from multiple providers to support intentional misuse) and dangerous interactions that can occur when mixing prescription and alcohol or illegal drugs. As part of this initiative, SAMHSA will educate at least 1,500 physicians in FY 2011 and provide training in at least eight states. (Action Item 2.2A)