ONDCP Blog
National Blueprint for Drug Policy Reform Released Today in Roanoke, VA
Posted by on July 9, 2014 at 8:50 AM ESTToday, we will unveil the latest update to President Obama’s plan for reducing drug use and its consequences, the 2014 National Drug Control Strategy. This Strategy, which continues to be shaped by the input of people across the country like you, rejects the notion that we can arrest and incarcerate our way out of the nation’s drug problem. Instead, it builds on decades of research demonstrating that while law enforcement should always remain a vital piece to protecting public safety, addiction is a brain disorder—one that can be prevented and treated, and from which people recover.
Data have shown that in several major U.S. counties, crime and substance use are linked. Most recently, we saw that in five counties, one-third or more of adult male arrestees tested positive for an illicit substance at the time of their arrest. Only one-quarter or fewer of all arrestees had ever participated in any outpatient drug or alcohol treatment and less than 30% had ever participated in any inpatient drug or alcohol treatment. Many of these men will be caught in a painful cycle of arrest, incarceration, substance use disorders, and re-arrest. Our prisons and jails are already overcrowded with people who desperately need compassionate, evidence-based treatment for the disease of addiction--not a jail cell.
The plan we released today calls for reforming our criminal justice system to find alternatives to incarceration – and effective interventions across the entire system to get people the treatment they need.
Here’s the problem: far too often, for people who need it most, the criminal justice system can seem like the only way to get help for a substance use disorder. That’s because until recently, prohibitively high costs and limited access to treatment put it out of reach for millions of people in need.
We know that only about 10 percent of people with a diagnosable substance use disorder actually receives treatment at a specialty facility. While several factors contribute to this abysmal statistic, much of that disparity is owed to a lack of healthcare coverage – and that’s about to change. Through a rule made possible by the Affordable Care Act, we are requiring insurers to treat substance use disorders in the same way they would any other chronic disease. Specifically, this new rule expands coverage of mental health and substance use disorder services to 62 million Americans.
The plan we released today calls on healthcare providers to prevent and treat addictive disorders just like they would treat any other chronic disorder, like diabetes or heart disease. It calls on law enforcement, courts, and doctors to collaborate with each other to treat addiction as a public health issue, not a crime.
We chose to release the 2014 Strategy in Roanoke because, in three important ways, it’s a microcosm of the policies our office has been promoting since 2009:
- Access to treatment, a focus on prevention, and compassion. Roanoke is home to one of the largest behavioral healthcare centers in the region. The center is co-located with a Drug Free Communities coalition, which prevents substance use among at-risk youth, and a program called Project Link, which helps opioid-dependent women and pregnant mothers get treatment and give birth to drug-free babies.
- Alternatives to incarceration. In 2011, the Roanoke Police Department worked with community and faith leaders in the Hurt Park neighborhood to shut down the open-air drug market operating there and drastically reduce violent crime in the area. As part of this intervention, community leaders came together to offer the low-level, non-violent drug offenders involved in the sweep a life-changing alternative: either face prosecution and lengthy sentences, or change your lives with the support of the community. In Roanoke, I met with one of those ex-offenders who is now employed full-time and caring for his family.
- Local solutions for local challenges. In a corner building in downtown Roanoke operates a community action center with roots in President Lyndon Johnson’s landmark anti-poverty legislation. Half a century ago, local leaders established what is now called Total Action for Progress (TAP), which operates 30 programs in the Roanoke Valley region aimed at improving employment opportunities at-risk youth, early childhood development, and re-entry and support services for veterans. I visited TAP to speak with young people and a veteran whose lives have been changed by these programs, and was inspired by their stories of hope.
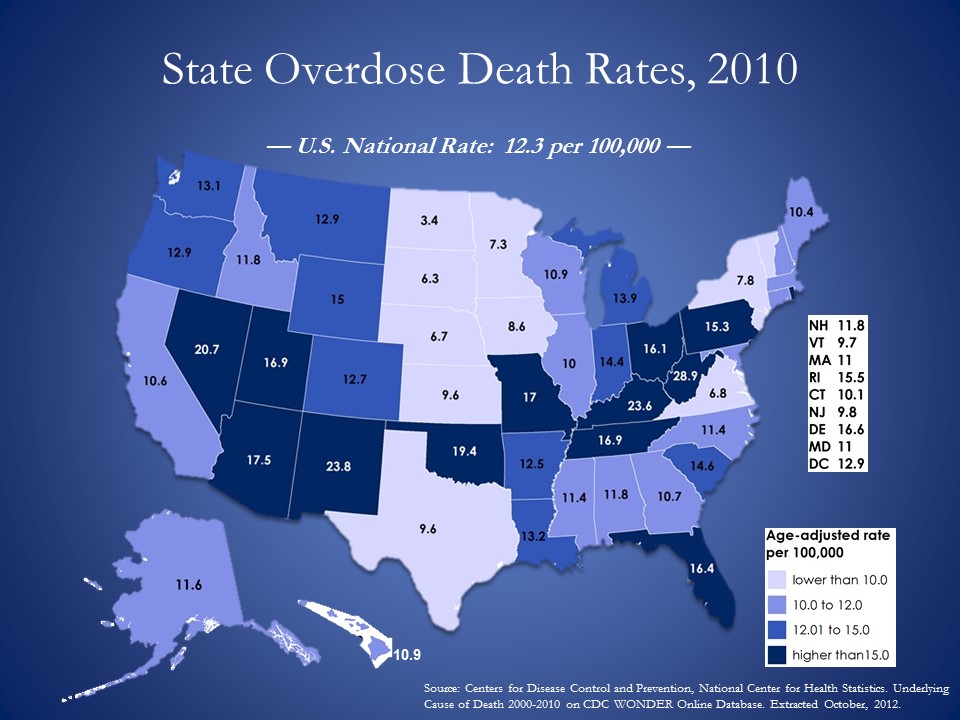
Like the rest of the country, Roanoke has seen a devastating rise in heroin and prescription painkiller abuse. According to the Centers for Disease Control and Prevention, drug overdose deaths surpass homicides and traffic crashes in the number of injury deaths in America.[1] In 2011, more than 110 Americans, on average, died from overdose every day. Prescription painkillers were involved in over 16,900 deaths that year. Heroin was involved in more than 4,300.[2]
In response to this opioid epidemic, this Strategy updates the President’s 2011 Prescription Drug Abuse Prevention Plan by calling for increased access to naloxone, a lifesaving overdose-reversal medication.
The widespread use of naloxone in the hands of law enforcement, firefighters and emergency medical personnel will save lives. It can also serve as a critical intervention point to get people into treatment and on the path to recovery.
Today, there are millions of Americans in recovery from substance use disorders who are healthy, responsible, and engaged members of their communities. The Strategy outlines steps to help lift the stigma associated with substance use disorders. It also works to reform the laws and regulations that impede recovery from substance use disorders, including those that place obstacles in the way of housing, employment, and obtaining a driver’s license or student loan because of a prior conviction for a drug-related offense.
The National Drug Control Strategy released today is rooted in the belief that illicit drug use is a public health issue, not just a criminal justice problem. As the innovative law enforcement and social support programs in Roanoke prove, this philosophy can reduce illicit drug use while building healthier, safer, more vibrant communities.
Learn more about what’s in the 2014 National Drug Control Strategy and sign up for email updates from my office.
Michael Botticelli is the Acting Director of National Drug Control Policy.
[1] National Center for Health Statistics/CDC, National Vital Statistics Report, Final death data for 2011 (June 2014).
[2] National Center for Health Statistics/CDC, National Vital Statistics, unpublished special tabulations (June 10, 2014).
Learn more aboutWhite House Summit on the Opioid Epidemic
Posted by on June 19, 2014 at 3:02 PM ESTToday, Acting Director Michael Botticelli hosted Attorney General Eric Holder, Vermont Governor Peter Shumlin, Director of National Institute on Drug Abuse Dr. Nora Volkow, and two panels of experts to address the national epidemic of opioid abuse.
The abuse of opioids, a group of drugs that includes heroin and prescription painkillers, has a devastating impact on public health and safety in this country. According to the Centers for Disease Control and Prevention (CDC), approximately 110 Americans, on average, died from drug poisoning every day in 2011.[i] Prescription drugs were involved in more than half of the 41,300 drug poisoning deaths that year, and opioid pain relievers were involved in nearly 17,000 of these deaths.[ii] There were about 4,400 drug poisoning deaths involving heroin. Drug poisoning deaths even outnumbered deaths from gunshot wounds or motor vehicle crashes.[iii]
Corrections to previously published number of deaths involving heroin: 2009 to 2011 should be 3,279, 3,038, and 4,397 respectively (for 2009 and 2010 to include deaths involving opium and a typo for 2011).
In his remarks, Attorney General Holder underscored the important role that law enforcement professionals play not only in reducing drug-related crime, but preventing overdose. Often, police officers are the first responders at the scene of an overdose, and their decisive action can mean the difference between life and death for an overdose victim.
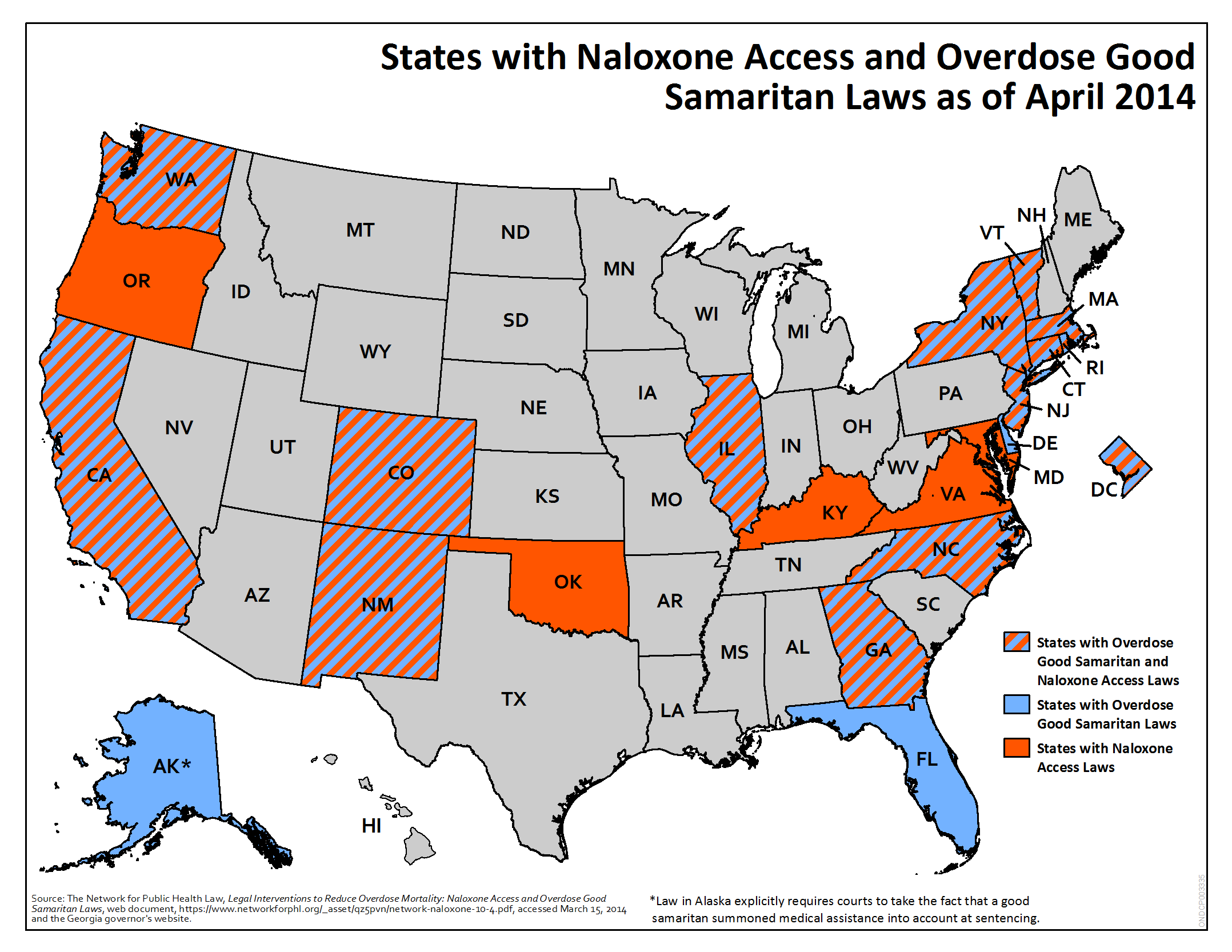
We join the Attorney General in encouraging first responders to carry the overdose-reversal drug naloxone. When administered quickly and effectively, naloxone immediately restores breathing to a victim in the throes of an opioid overdose. Used in concert with “Good Samaritan” laws, which grant immunity from criminal prosecution to those seeking medical help for someone experiencing an overdose, naloxone can save lives. The map below shows which states currently have laws which increase access to naloxone and encourage witnesses to an overdose to call 911:
Governor Shumlin, who previously dedicated his entire State of the State address to the opioid crisis in Vermont, outlined the steps his administration is taking to prevent and treat substance use disorders.
Dr. Nora Volkow provided an overview of the groundbreaking advances we’ve made over the past several decades in the study of addiction – a progressive disease of the brain that can be prevented, treated and recovered from. Watch her discuss the disease of addiction:
The opioid epidemic has already brought heartbreak to too many families across the country – but we’re not powerless to stop it. You can help – right now – by spreading the word about how to save a life and where to seek treatment.
Missed the summit? Watch videos of the summit here:
Rx Drug and Heroin Epidemic in the States
Presentations:
Robert Morrison
Executive Director, National Association of State Alcohol and Drug Abuse Directors (NASADAD)Panel I - Prevention, Intervention and Treatment
Presentations:
Dr. Hillary Kunins
Acting Executive Deputy Commissioner, Division of Mental Hygiene, Assisting Commissioner for the Bureau of Alcohol and Drug Use, New York City Department of Health and Mental Hygiene (DOHMH)Dr. Traci Green
Assistant Professor of Emergency Medicine and Epidemiology, Brown UniversityDr. Josh Sharfstein
Secretary, Maryland Department of Health and Mental HygienePanel II: Overdose and Infectious Disease Prevention
Presentations:
Nancy Hale
Program Director, Operation UNITEDr. Michelle Lofwall
Associate Professor, Departments of Psychiatry and Behavioral Science, Center on Drug and Alcohol Research, University of Kentucky College of MedicineDr. Ed Bernstein
Professor and Vice Chair for Academic Affairs, Emergency Medicine, Boston University School of Medicine
[i] National Center for Health Statistics/CDC, National Vital Statistics Report, Final death data for each calendar year (June 2014)..
[ii] National Center for Health Statistics/CDC, National Vital Statistics Report, Final death data for each calendar year (June 2014)..
[iii] National Center for Health Statistics/CDC, National Vital Statistics Report, Final death data for each calendar year (June 2014).
Learn more aboutJoin the Discussion: Summit on Opioids on June 19
Posted by on June 16, 2014 at 5:40 PM ESTThe abuse of opioids – a group of drugs that includes heroin and prescription painkillers – is devastating public health and safety in communities across the nation. While the Obama Administration has been leading a comprehensive response to the prescription drug problem for more than four years, the recent uptick in heroin use across the country, and the increasing number of overdose deaths, requires a new approach.
Michael Botticelli, Acting Director of National Drug Control Policy, will be joined by Eric Holder, U.S. Attorney General, Peter Shumlin, Governor of Vermont, Nora Volkow, Director of the National Institute on Drug Abuse, and other public health and government leaders to discuss the scope of the epidemic and strengthen collaborations across government to ensure we’re doing everything we can do prevent substance use disorders, reduce overdose deaths and treat those who are struggling with addiction.
Please join us for this important conversation. Here’s how:
Watch live from 9 a.m. to 12:30 p.m. on Thursday, June 19 at whitehouse.gov/live.

Share your story and ask questions on Twitter using #OpioidSummit, and follow @ONDCP for live updates.
Sign up for email updates for the latest news in drug policy.
Learn more aboutHow a Vermont Hospital Fights the American Opioid Epidemic
Posted by on May 9, 2014 at 1:35 PM ESTOver the course of my more than 20 years as an emergency physician, I have seen thousands of patients with painful conditions. During that same time, I have witnessed the remarkable evolution of modern pain medication – its potential and its pitfalls. We can now help patients manage both short-term and long-term pain. Yet, while medications – particularly opioids – have helped us heal patients, we have also seen their detrimental effects, chief among them addiction.
Opioids can be very helpful for patients with conditions such as broken bones and kidney stones, and they are also useful after many types of surgery. They may also be used to treat those with chronic pain – people who experience pain carrying out normal, daily functions of life that others take for granted. Used for short periods of time at the proper dosage, opioids are safe medications and excellent choices for a wide variety of acute painful conditions.
While opioids work well for pain control, they have a number of potentially serious side effects: They can hinder or stop breathing, cause constipation, result in drowsiness, and act as central nervous system depressants. That’s why your doctor tells you it is not safe to drive after taking opioids.
Another devastating side effect is addiction. The body develops a tolerance to opioids and, after only a couple of weeks, may require higher doses to control pain. Over time, increasing doses of opioids may be needed to manage the same level of pain. Patients may develop dependence – their bodies will crave it. They will exhibit a strong desire or compulsion to take the drug for reasons beyond simple pain control. At this stage, if they stop taking opioids, they will experience withdrawal. This is how opioid use can lead to addiction and all its inherent problems for the individual and society.
As providers, our responsibility is to carefully manage the side effects of opioid therapy. Dependence, tolerance, and addiction must be discussed with patients, and a careful well-planned strategy is crucial for their extended use of opioids.
That is exactly what we are doing at Fletcher Allen Health Care in Burlington, Vermont. Recently, providers and pain management experts from multiple specialties (Anesthesia, Emergency Medicine, Family Medicine, Internal Medicine, and Surgery) converged to standardize how we care for patients with painful conditions and to develop best practices for our patients.
What did we do? Here is an overview:
- Systems Approach. We built standardized protocols so that patients will get similar treatment in various settings. We believe this standardization will help our patients and providers. There will be clear, defined expectations and goals for treating our patients’ pain.
- New Rules & Tools. We use processes and tools such as pain agreements with patients and surveys to assess how patients are functioning with their pain and to measure their risk for addiction.
- Defining Maximum Daily Dosage. We are one of the first hospitals in the country to define the maximum daily dose of opioids. Research shows that beyond certain doses, patients experience no additional benefit. We know that very high doses of opioids increase the risk of dangerous side effects but offer no additional pain control.
This approach helps ensure that we are more reliable and consistent in our approach to pain in our patients and that our patients will know what to expect from their providers.
Gil Kerlikowske, then-Director of ONDCP, recently visited Fletcher Allen Health Care to discuss our new approach and tools. He lauded our systems-level strategy and our standardized protocols.
I believe that the current dialogue in Vermont and elsewhere on how to better manage opioid abuse will be productive and lead to changes across the country in how these drugs are prescribed and how acute and chronic pain is managed. Fletcher Allen Health Care is on the leading edge of this transition and could be a model for other health systems managing this complex issue. I hope that sharing our practices here is the first step toward being that model.
Stephen M. Leffler, M.D., is the Chief Medical Officer at Fletcher Allen, former Medical Director of the Emergency Department, and has been a practicing physician for 20 years. He grew up in Brandon, Vermont.
Learn more aboutActing Director Botticelli Addresses OAS Anti-Drug Group
Posted by on May 6, 2014 at 2:43 PM ESTOn May 1, ONDCP Acting Director Michael Botticelli spoke at the 55th regular session of the Inter-American Drug Abuse Control Commission (CICAD) in Washington, D.C. The 34 Member Nations from the Organization of American States (OAS) gathered to discuss an array of public health and drug policy issues, including drug courts and other alternatives to incarceration and the growing challenge of local distribution of drugs within Latin America, a practice known as “micro-trafficking” in Colombia, which is serving as the CICAD Chair.Dr. Wilson Compton, Deputy Director of the National Institute on Drug Abuse, joined Acting Director Botticelli on a panel to discuss “Health Issues and Policies related to Cannabis.” Acting Director Botticelli discussed the disease of addiction, the expanding access to drug treatment under the Affordable Care Act, and Federal monitoring of state marijuana laws in Colorado and Washington. His remarks were followed by Dr. Compton’s detailed presentation on the current scientific understanding of marijuana’s short- and long-term effects on the brain and body.Read Acting Director Botticelli's remarks and sign up for regular updates from our office.Learn more aboutMark Your Calendar: April 26th is National Prescription Drug Take-Back Day
Posted by on April 22, 2014 at 10:10 AM ESTThis Earth Day, we encourage all Americans to take action to protect the planet while protecting their health by making plans to participate in National Prescription Drug Take-Back Day this Saturday, April 26th from 10 a.m. to 2 p.m.
Many prescription drugs that lie unused in home medicine cabinets are highly susceptible to diversion, misuse, and abuse. Research has shown that about 70 percent of those who abused prescription pain relievers in the past year obtained them from family or friends – and often from the home medicine cabinet – the last time they used them.
The environmentally responsible disposal of these drugs is a pillar of the Obama Administration’s plan to prevent prescription drug abuse. While you may have heard flushing your old pills down the toilet is the best way to dispose of them, that’s not necessarily true. Medicines that go down the drain end up in our water supply, where they can damage the environment. Saturday’s Take-Back Day is a convenient opportunity to get rid of unneeded medicine and prevent these drugs from entering our water supply.
Locate a collection site near you.
In 2010, approximately 100 people died every day from opioid drug overdoses, and prescription opioids were involved in 43 percent of those overdose deaths. Opioid drug abuse has devastated thousands of communities across the country. As ONDCP Acting Director Michael Botticelli recently put it, “This is an epidemic of the medicine cabinet.”
If you have unneeded or expired prescription drugs at home, we strongly encourage you to drop them off at a safe, legal collection site in your neighborhood on Saturday, April 26, as part of the Drug Enforcement Administration’s (DEA) National Prescription Drug Take-Back Day.
Take-Back Days are vital to supporting the Administration’s efforts to reduce the accessibility of illegal drugs and combat substance abuse. They provide a responsible and convenient way for people to properly dispose of their prescription drugs, and they help educate the public about the potential for their abuse. Since its launch in September 2010, the Take-Back Day initiative has resulted in the collection and proper disposal of 3.4 million pounds of medication – including 647,211 pounds collected during last year’s event.
The Secure and Responsible Drug Disposal Act, passed by Congress in 2010, requires DEA to draft regulations that will provide for more convenient disposal of prescription drugs. The new rule is expected to be issued before the end of the year and paves the way for an easier and environmentally responsible means of disposal in communities across the country.
This year’s Take-Back Day will occur nationwide from 10 a.m. to 2 p.m. on Saturday, April 26th. Disposal sites will be set up in all 50 states, Washington, D.C., and U.S. territories. Find a take-back location near you today.
Learn more aboutAnnouncing Another Tool to Save Lives
Posted by on April 3, 2014 at 3:38 PM ESTToday, the Food and Drug Administration approved a new drug that will build upon our work to turn back the tide of our nation’s overdose epidemic. This new product – Evzio - works by delivering a single dose of naloxone via a hand-held auto-injector that can be carried in a pocket or stored in a medicine chest for rapid access by first responders and caregivers responding to an opioid overdose.
Why is this so important? Naloxone is a lifesaving overdose reversal drug that rapidly reverses the effects of opioid overdose and is currently the standard treatment for overdose. This product is easier to administer than naloxone products that must be administered via syringe and is similar to an epi-pen.
The FDA’s approval of another overdose reversal drug could not come at a more urgent time. Drug overdose deaths, driven largely by prescription drug overdose, are now the leading cause of injury death in the United States – surpassing motor vehicle crashes.
There are no silver bullet solutions to our nation’s overdose epidemic. Prevention, treatment, and smart on crime efforts each play a vital role in protecting public health and safety in America. Working together, we can save lives and strengthen our nation’s ability to prosper.Learn more aboutJoin Us for Launch of the Updated Viral Hepatitis Action Plan on Thursday, April 3
Posted by on March 27, 2014 at 3:18 PM ESTThis is a cross-post from AIDS.gov. The original post can be found here.Next Thursday, April 3, 2014, we will launch the three-year update (2014-2016) of the Action Plan for the Prevention, Care and Treatment of Viral Hepatitis. The plan provides a framework around which both federal and nonfederal stakeholders from many sectors can engage to strengthen the nation’s response to viral hepatitis. The event will be streamed online live from HHS headquarters in Washington, DC, so that as many federal, state, and community-based partners across the country as possible can participate.Please join us for the launch event, which can be viewed live online at www.hhs.gov/live on Thursday, April 3, 2014 from 12:00 PM – 3:00 PM (Eastern). Invite others to watch with you so you can talk about how you can work together in your community to improve viral hepatitis prevention, screening, and treatment.The launch event is the culmination of efforts by colleagues from across the Department of Health and Human Services as well as at the Departments of Justice, Housing and Urban Development, and Veterans Affairs who have worked within their respective agencies and offices as well as with one another to develop this framework for focused activity by both federal and nonfederal stakeholders. Federal colleagues have identified more than 150 important actions their agencies and offices will undertake between 2014 and 2016 across six priority areas.More than 100 nonfederal stakeholders shared thoughts, general principles, and specific recommendations that helped to shape the renewed plan over the course of its development. A notable feature of the plan is a list of potential opportunities for non-federal stakeholders that would promote successful implementation. These implementation opportunities make it crystal-clear that achieving the goals of this national plan will require the time, talent, and energy of a broad mix of partners from across all sectors of society. The launch event will feature two panels – governmental and community – that will discuss, in practical terms, implementation challenges and opportunities as well as remarks by Assistant Secretary for Health Howard Koh, MD, MPH.The updated plan organizes actions around the following six priority areas:
1: Educating Providers and Communities to Reduce Viral Hepatitis-related Health Disparities
Confront viral hepatitis by breaking the silence.2: Improving Testing, Care, and Treatment to Prevent Liver Disease and Cancer
Take full advantage of existing tools.
3: Strengthening Surveillance to Detect Viral Hepatitis Transmission and Disease
Collect accurate and timely information to get the job done.
4: Eliminating Transmission of Vaccine-Preventable Viral Hepatitis
Take full advantage of vaccines that can prevent hepatitis A and B.
5: Reducing Viral Hepatitis Associated with Drug Use
Stop the spread of viral hepatitis associated with drug use.
6: Protecting Patients and Workers From Health Care-Associated Viral Hepatitis
Quality health care is safe health care
The day of the launch event, the updated Viral Hepatitis Action Plan and other information will be posted to the Viral Hepatitis Action Plan page hosted by aids.gov.
Please join us for this event to learn more and help us kick-off this renewed plan that can improve our nation’s response to viral hepatitis. Together, we can prevent new infections and save many lives.
Dr. Ronald Valdiserri is the Deputy Assistant Secretary for Health, Infectious Diseases and Director, Office of HIV/AIDS and Infectious Disease Policy.
Learn more aboutRecovery Movement Endorsed by United Nations
Posted by on March 25, 2014 at 3:18 PM ESTA resolution on the importance of recovery proposed by the United States at the 57th session of the Commission on Narcotic Drugs (CND) was approved on March 21st in Vienna, Austria. This resolution marks the first time in the more than 50-year history of the global anti-drug regime that the concept of recovery was formally accepted and supported by United Nations Member States.
Acting Director of National Drug Control Policy Michael Botticelli said: “This is a historic moment. For too long, the recovery movement has gone without a voice in the global conversation about drug policy. Talking about recovery, exchanging experiences and programs, and sharing successes at international forums like the Commission on Narcotic Drugs is a critical part of a public health approach to preventing and treating substance use disorders and reducing the global drug problem. The resolution codifies the commitment of countries to decrease the stigma associated with substance use disorders and to address them like other chronic health conditions.”
Mr. Botticelli further noted his appreciation for the support for the resolution provided by many nations, including Australia, Canada, Germany, Italy, New Zealand, and the United Kingdom, and also for the assistance and advice provided by the many American and international non-governmental organizations that were present in Vienna for the CND.
The resolution, entitled Supporting Recovery from Substance Use Disorders, recognizes that substance use disorders can result in chronic relapsing conditions and that recovery support initiatives help to prevent relapse, facilitate re-entry into treatment when needed, and promote long-term recovery outcomes. The resolution also calls for an end to stigma, marginalization, and discrimination against those in recovery; promotes international exchanges on best practices related to recovery support initiatives; and encourages the United Nations Office on Drugs and Crime (UNODC) to disseminate globally information about evidence-based recovery support initiatives. The resolution, which was co-sponsored by a number of countries, was approved at the UNODC meeting on Friday, March 21, 2014.
Learn more aboutPresident Obama Announces Douglas M. Brooks, MSW, as Director of the Office of National AIDS Policy
Posted by on March 24, 2014 at 2:12 PM ESTToday, President Obama announced the appointment of Douglas M. Brooks, MSW, as the Director of the White House Office of National AIDS Policy (ONAP). A leading HIV/AIDS policy expert, Douglas most recently served as Senior Vice President for Community, Health, and Public Policy at the Justice Resource Institute (JRI). As the Director of ONAP, he will lead the Administration’s work to reduce new HIV infections, improve health outcomes for people living with HIV, and eliminate HIV health disparities in the United States.
“Douglas’s policy expertise combined with his extensive experience working in the community makes him uniquely suited to the task of helping to achieve the goal of an AIDS-free generation, which is within our reach,” President Obama said. “I look forward to having him lead our efforts from the White House.”
A component of the White House Domestic Policy Council, ONAP coordinates the ongoing implementation of the National HIV/AIDS Strategy and the HIV Care Continuum initiative, while working together with public and private partners to advance the federal response to HIV/AIDS. ONAP also works with the White House National Security Council, the State Department’s Office of the Global AIDS Coordinator, and international bodies to ensure that America’s response to the global pandemic is fully integrated with prevention, care, and treatment efforts around the world. Through the U.S. President's Emergency Plan for AIDS Relief (PEPFAR) initiative, the U.S. has made enormous progress in responding to the global HIV/AIDS pandemic, working with countries heavily impacted by HIV/AIDS to help expand access to treatment, care, and prevention.
Brooks, a person living with HIV, was most recently the Senior Vice President for Community, Health, and Public Policy at JRI, a health and human service agency based in Boston. He served as executive director of the Sidney Borum Jr. Community Health Center at JRI, has managed programs in urban and rural environments and has served as a consultant to domestic and international governments and non-governmental organizations assisting their efforts to serve populations living with and at greatest risk for HIV/AIDS. Brooks was a Visiting Fellow at the McCormack School Center for Social Policy at the University of Massachusetts, Boston and was Chair of the Board of Trustees of AIDS United in Washington, DC.
In 2010, Brooks was appointed to the Presidential Advisory Council on HIV/AIDS (PACHA) and served as its liaison to the CDC/HRSA Advisory Committee and successfully led those bodies to achieve the tasks assigned to them in the National HIV/AIDS Strategy. He has directly managed federally funded programs, meeting or exceeding targets for Ryan White projects, CDC Prevention for African American/Black youth, a HRSA Special Project of National Significance (SPNS), and a HOPWA SPNS. Brooks received a Master of Social Work degree from Boston University and is a licensed clinical social worker.
Learn more about
- &lsaquo previous
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- …
- next &rsaquo



